Sedation explained
Sedation is usually given into your vein (IV or intravenous), but can sometimes be given by mouth (oral) or through a face mask.
What is intravenous sedation?
Intravenous sedation is when a sedative (sedation medicine) is injected into your bloodstream (vein) through a drip (tube) to relax you.
‘Sedationist’ is the name given to the healthcare professional who does this.
They are trained in giving the right amount of sedative and managing any side effects. In the operating theatre, the sedationist is usually an anaesthetist. In other settings, this may be a nurse, surgeon or other trained practitioner. Your sedationist will stay with you all the time during your treatment.
There are three different levels of intravenous sedation. They are called ‘minimal’, ‘moderate’ (sometimes also called conscious sedation) and ‘deep’ sedation.
■ Minimal sedation – the sedationist will give you a small amount of sedative. You will feel relaxed and less worried by what is happening around you, but you will be awake and able to talk normally. You are likely to remember having your treatment, but not all the detail. Minimal sedation should not affect your breathing.
■ Moderate sedation (conscious sedation) – the sedationist will give you a little more sedative(s) so you will feel very relaxed and drowsy. Importantly though, your sedationist can still talk with you and you will still be able to follow simple instructions. You may remember some parts of your treatment. Moderate sedation should not affect your breathing.
■ Deep sedation – the sedationist will give you a higher dose of one or more drugs that will make you sleep during most of your treatment. Your doctor will not expect to talk to you during your treatment. Your breathing may be affected and your sedationist will watch and help you if needed. You may sometimes remember part of your treatment. In the UK, deep sedation must be administered by staff who have the level of training and skill of an anaesthetist.
What is oral sedation?
This can sometimes be useful to relax very anxious people before a general anaesthetic, but it is usually not enough to relax you during a procedure on its own. It takes a while to work and it can be difficult to get the right dose as it varies between people.
Please do not ask your GP to prescribe oral sedatives for you to take before you come into hospital, unless you have already signed your consent form, as it can affect your thinking and judgement.
It is important that you can think clearly when you meet with your doctor to discuss the risks and to sign a form to state that you agree to have the operation or procedure.
What are the differences between sedation and general anaesthesia?
The main differences between sedation and general anaesthesia are:
■ your level of consciousness
■ the need for equipment to help support your breathing
■ possible side effects.
With minimal and moderate sedation you feel drowsy, comfortable, sleepy and relaxed, but you remain conscious throughout the procedure.
With general anaesthesia you are completely unresponsive and unconscious during the procedure.
Deep sedation is between the two.
What treatments can be carried out under intravenous sedation?
Many minor treatments can be undertaken with intravenous sedation. A few examples include:
■ skin or breast biopsies
■ minor repair to fractured bones
■ minor surgery to the skin, hand or foot
■ procedures to help diagnose problems with the stomach (endoscopy), the lung (bronchoscopy), the colon (colonoscopy) or the bladder (cystoscopy)
■ removal of teeth or other dental treatment
■ eye operations, such as cataract removal.
What are the benefits of intravenous sedation?
■ It is quick acting and the dose can be adjusted so you get just the right amount.
■ It allows you to be more relaxed during your treatment. It may also mean that you remember very little about your treatment afterwards.
■ For some procedures, it avoids the need for a general anaesthetic which may be unsuitable for patients with some medical problems.
■ It usually has fewer side effects than a general anaesthetic.
■ Recovery is quicker than after a general anaesthetic, so you can usually go home within an hour of your treatment if you feel well.
What are the risks of intravenous sedation?
■ Your breathing rate may become slow. This is common in deep sedation, but is a risk whenever sedation is used. The sedationist is skilled in monitoring you and can assist your breathing if required.
■ It is common for your blood pressure to drop, but the sedationist is trained in treating this too.
■ Feeling sick or vomiting can happen, but is uncommon.
■ Any allergic reaction to the sedation drugs is very rare.
■ You may have a small bruise where your cannula was placed or attempted.
■ Afterwards you may feel less steady on your feet and you may be at higher risk of falling, especially if you are elderly.
■ Sedation can affect your judgement and memory for up to 24 hours.
What are the alternatives to sedation?
■ A general anaesthetic: you will be fully unconscious throughout and have no memory of the procedure.
■ Local anaesthetic without any sedation: you will be fully awake during your treatment, but will be comfortable. A screen can be placed to stop you seeing the procedure.
Who decides whether I can have sedation?
You can discuss the option of sedation with your doctor or nurse at the time of assessment. If it hasn’t been offered, you can always ask to see if it is possible to have it.
If you are at higher risk from existing medical conditions, your doctors will discuss the options with you and you can reach a decision together.
I’m having sedation, what should I do before I come to the hospital?
■ If you have people that you look after, for example children or old people, you will need to plan for someone else to look after them until the next day.
■ A capable adult will need to take you home by car or taxi – ideally not public transport. As the effects of sedation can last up to 24 hours, they should stay overnight to look after you.
■ Take all your medicines to hospital with you, including any inhalers you use.
■ If you have an illness, a cold or you are pregnant, please contact your hospital as it may not be safe to have sedation. Your treatment may have to be re-arranged.
■ Let your doctor know on the day of the procedure if you are breastfeeding.
■ Remove all makeup – including nail varnish and jewellery – before coming to hospital. You may wear a wedding band.
■ Bring some loose clothing, such as a dressing gown or a fleece, to keep you comfortable and warm. Wear flat shoes that are easy to put on.
Can I eat and drink before my treatment?
The clinic or hospital will give you instructions on when to stop eating and drinking.
You will usually be asked to stop eating six hours before your treatment, but you may drink clear fluids up to two hours before your treatment. Clear fluids you will be allowed to drink include water, diluted juice (no bits) and black tea or coffee (no milk or cream).
If you have diabetes, you should ask for specific instructions about when you should take your medication and stop eating food.
What will happen before my treatment?
You will usually change into a gown. When you go to the procedure room, your sedationist will attach some monitoring equipment to you. The equipment used will depend upon what procedure and type of sedation you are having, but will usually include:
■ a blood pressure cuff on your arm
■ leads on your upper chest to record your heart rhythm
■ a clip on your finger to measure your oxygen levels
■ a thin plastic tube that measures the amount of carbon dioxide that you breathe out. This is usually attached to an oxygen mask.
How is intravenous sedation given?
■ The sedation is given through a drip (cannula) which is put into a vein in your arm or the back of your hand. More can be given as you need it during the procedure. In deep sedation you will usually have a drug given continuously into your vein.
■ You will usually have oxygen to breathe from a plastic tube sitting just inside your nose, or through a face mask.
What does sedation feel like?
This will vary between people, depending on how much of the drug they are given. In deep sedation you will be asleep, but in light sedation you usually feel pleasantly relaxed.
When we asked some patients what it felt like, some answers were:
‘I felt very spaced out and dreamy’
‘I thought I had been awake during it all but I must have drifted off at times as suddenly it was an hour later’
‘I felt really relaxed and happy’
‘It was weird – I felt very detached from what was happening around me.’
When can I go home?
■ If you have light or moderate sedation, you can usually go home within an hour of your treatment.
■ If you have deep sedation, your recovery will likely take one to two hours. When you can go home may often depend on recovery from the procedure itself.
Are there any important instructions for afterwards?
■ As previously stated, a capable adult will need to take you home by car or taxi – ideally not public transport – and remain with you overnight. If arrangements have not been made for someone to accompany you after treatment, you may not be able to go home after the procedure.
■ Sedation may make you unsteady on your feet. Please be careful on stairs and have somebody with you if you feel unsteady.
■ Your decision making may be affected for up to 24 hours after your treatment, so you should not make any important decisions during that time. Be careful if using social media.
■ You should not return to work, look after dependants, drive, cook or operate any machinery for 24 hours. It can take 24 hours for the drugs to leave your body.
■ You should not take any alcohol or sleeping tablets for 24 hours after the procedure.
■ Your doctor will give written instructions about further treatment to follow at home.
■ The hospital will give you a contact telephone number to call if you feel unwell at home.
■ If after the procedure you are concerned, feel unwell, or cannot find this number, you can call your GP, ring 111, or go to your local accident and emergency department with a capable adult if necessary.
Questions you may like to ask your anaesthetist
1 Who will give my sedation?
2 Do you recommend sedation or a general anaesthetic?
3 Do I have any special risks?
4 When should I stop eating and drinking before my sedation?
5 What time should I arrange to be collected?
Side-effects, complications and risks
In modern anaesthesia, serious problems are uncommon. Risk cannot be removed completely, but modern drugs, equipment and training have made anaesthesia a much safer procedure in recent years.
Anaesthetists take a lot of care to avoid all the risks outlined in this section. Your anaesthetist will be able to give you more information about any of these risks and the precautions taken to avoid them.
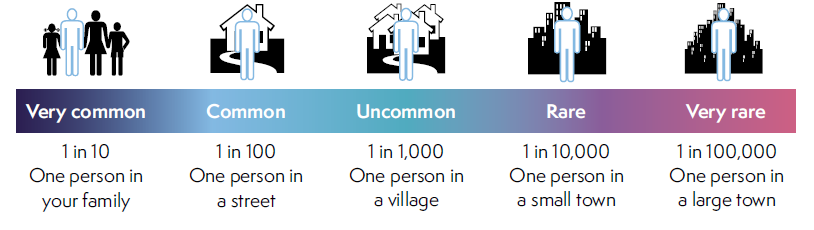
People vary in how they interpret words and numbers. This scale is provided to help.
You can also find out more information from the patient information pages on the College website: http://www.rcoa.ac.uk/patientinfo
Additional resources
Caring for someone who has had a general anaesthetic or sedation (www.rcoa.ac.uk/patientinfo/sedation)
Standards for Conscious Sedation in the Provision of Dental Care. The Royal College of Surgeons of England and the Royal College of Anaesthetists. RCoA, London 2015 (www.rcoa.ac.uk).
Guidance on the Provision of Sedation Services. RCoA, London 2016 (www.rcoa.ac.uk).
Safe Sedation Practice for Healthcare Procedures: Standards and Guidance. Academy of Medical Royal Colleges. AoMRC, London 2013 (bit.ly/2m3rUfc).
You can find more information leaflets on the College website www.rcoa.ac.uk/patientinfo. The leaflets may also be available from the anaesthetic department or pre-assessment clinic in your hospital.
Risks associated with your anaesthetic
The following are leaflets about specific risks associated with having an anaesthetic or an anaesthetic procedure. They supplement the patient information leaflets listed above and are also available via the College website: www.rcoa.ac.uk/patientinfo/risks
■ Feeling sick.
■ Sore throat.
■ Shivering.
■ Damage to teeth, lips and tongue.
■ Damage to the eye during general anaesthesia.
■ Post-operative chest infection.
■ Becoming confused after an operation.
■ Accidental awareness during general anaesthesia.
■ Serious allergy during an anaesthetic (anaphylaxis).
■ Headache after a spinal or epidural injection.
■ Nerve damage associated with having an operation under general anaesthetic.
■ Nerve damage associated with a spinal or epidural injection.
■ Nerve damage associated with peripheral nerve block.
■ Equipment failure.
■ Death or brain damage.

