Your spinal anaesthetic
Having a spinal anaesthetic
■ what a spinal anaesthetic is
■ how it works, and
■ why you could benefit from having one for your operation.
For many operations, patients receive a general anaesthetic, which produces a state of controlled unconsciousness during the operation.
As an alternative, for operations below the waist, you can have a spinal anaesthetic. This is when an injection is placed in your back, which makes you numb from the waist downwards. This means you cannot feel the operation being done. Depending on your medical condition and the operation you are having, this may be safer or more comfortable for you.
During your spinal anaesthetic, you can be:
■ fully awake
■ sedated – drugs make you relaxed and sleepy but not unconscious
■ fully anaesthetised (unconscious).
Your anaesthetist can help you decide which of these would be best for you.
Almost any operation below the waist is suitable for a spinal anaesthetic. Depending on your personal health, there may be benefits to you from having a spinal anaesthetic. Your anaesthetist is there to discuss this with you and help you make a decision as to what suits you best.
A spinal anaesthetic is often used for:
■ orthopaedic surgery on joints or bones of the leg
■ groin hernia repair, varicose veins, haemorrhoid surgery (piles)
■ vascular surgery: operations on the blood vessels in the leg
■ gynaecology: prolapse repairs and some kinds of hysterectomy
■ obstetrics: caesarean section
■ urology: prostate surgery, bladder operations, genital surgery.
What is a ‘spinal’?
A local anaesthetic drug is injected through a needle into the middle of your lower back, to numb the nerves from the waist down to the toes for two to three hours. Other drugs may be injected at the same time that prolong pain relief for many hours.
How is the spinal performed?
1 Your anaesthetist will discuss the procedure with you beforehand on the ward.
2 In the anaesthetic room, you will meet an anaesthetic assistant who will stay with you during your time in the theatre.
3 The spinal may be done in the anaesthetic room or in the operating theatre.
4 Your anaesthetist will use a needle to insert a thin plastic tube (a ‘cannula’) into a vein in your hand or arm.
5 You be helped into the correct position for the spinal. You will either sit on the side of the bed with your feet on a low stool or you will lie on your side, curled up with your knees tucked up towards your chest.

6 The anaesthetic team will explain what is happening, so that you are aware of what is taking place ‘behind your back’.
7 The anaesthetist will give you the spinal injection. Local anaesthetic is used in the skin to make the spinal injection more comfortable. A nurse or healthcare assistant will support and reassure you during the injection.
8 As the spinal begins to take effect, your anaesthetist will test its effectiveness.
What will I feel?
A spinal injection is often no more painful than having a blood test or having a cannula inserted. It may take several minutes to perform.
■ Most patients feel no abnormal sensation but as the injection is made you may feel pins and needles or a sharp pain in one of your legs – if you do, try to remain still, and tell your anaesthetist.
When the injection is finished, you will be asked to lie flat. The spinal works quickly and is usually effective within five to ten minutes.
■ To start with your skin feels warm, then numb to touch and then gradually your leg muscles become weak.
■ When the injection is working fully, you will be unable to move your legs or feel any pain below the waist.
Testing the block
■ Your anaesthetist may use a range of simple tests to see if the block is working properly.
■ He/she may spray a very cold liquid on your skin and ask you what you can feel. He/she may ask you to distinguish between cold and wet sensations from the spray. Please try and simply describe what you can feel and where. If the feeling of cold is lost at this early stage, this is a good sign that the spinal will work well for the surgery.
■ He/she may also ask you to try and move your legs. If you cannot move them, then the spinal is working very well. If you still have some movement, the anaesthetist will decide if this is significant.
Only when the anaesthetist is satisfied that the anaesthetic has taken effect will he/she allow the surgery to begin.
During the operation
■ In the operating theatre, a full team of staff will look after you. If you are awake, they will introduce themselves and try to put you at your ease.
■ You will be positioned for the operation. Please tell your anaesthetist if there is something simple that will make you more comfortable, such as an extra pillow or armrest.
■ You may be given oxygen to breathe via a lightweight, clear plastic mask, to improve oxygen levels in your blood.
■ You will be aware of the ‘hustle and bustle’ of the operating theatre when you come in. Once surgery starts, noise levels drop. You will be able to relax, with your anaesthetist looking after you.
■ You can listen to music if you wish during the operation. Feel free to bring your own music, with headphones.
■ You can communicate with the anaesthetist during the operation. If an operating camera is used, and there is an extra screen, you may be able to watch the operation on the screen, if you want to.
■ Alternatively, you may be receiving sedation during the operation. You will be relaxed and sleepy but not unconscious.
However, you may still need a general anaesthetic if:
■ your anaesthetist cannot perform the spinal to his/her satisfaction
■ the spinal does not work adequately in the area of the operation
■ the surgery is more complicated or takes longer than expected.
After the spinal
■ It takes one to four hours for sensation (feeling) to return to the area of your body that is numb. You should tell the ward staff about any concerns or worries you may have.
■ As sensation returns, you may experience some tingling in the skin as the spinal wears off. At this point, you may become aware of some pain from the operation site and you should ask for more pain relief before the pain becomes too obvious.
■ You may be unsteady on your feet when the spinal first wears off. Please ask for help from your nurse when you first get out of bed.
■ You can normally drink fluids within an hour of the operation and may also be able to eat a light diet.
Why have a spinal?
Advantages compared to having a general anaesthetic There may be:
■ less risk of a chest infection after surgery
■ less effect on the lungs and the breathing
■ excellent pain relief immediately after surgery
■ less need for strong pain-relieving drugs. This is because the local anaesthetic and any pain relief drugs given in the spinal reduce the need for pain relief medicines given in other ways, which tend to have many more side effects, including nausea, confusion, drowsiness and constipation
■ less sickness and vomiting
■ earlier return to drinking and eating after surgery
■ less risk of becoming confused after the operation, especially if you are an older person.
Side effects and complications
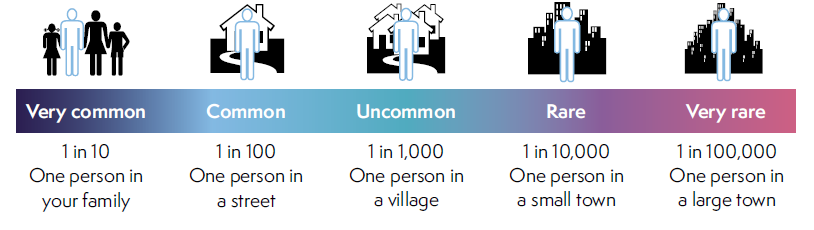
As with all anaesthetic techniques, there is a possibility of unwanted side effects or complications.
Very common and common side effects
These may range from trivial to unpleasant, but can be treated and do not usually last long.
■ Low blood pressure – as the spinal takes effect, it can lower your blood pressure. This can make you feel faint or sick. This will be controlled by your anaesthetist with the fluids given through your drip and by giving you drugs to raise your blood pressure.
■ Itching – this can occur as a side effect of using morphine-like drugs in combination with local anaesthetic drugs in the spinal anaesthetic. If you experience itching, it can be treated. Please let the staff know if you are itchy.
■ Difficulty passing water (urinary retention) – you may find it difficult to empty your bladder normally for as long as the spinal lasts. Your bladder function returns to normal after the spinal wears off. You may require a catheter to be placed in your bladder temporarily, while the spinal wears off and for a short time afterwards. Bowel function is not affected by the spinal.
■ Pain during the injection – if you feel pain in places other than where the needle is – you should immediately tell your anaesthetist. This might be in your legs or bottom, and might be due to the needle touching a nerve. The needle will be repositioned.
■ Headache – there are many causes of headache after an operation, including the anaesthetic, being dehydrated, not eating and anxiety. Most headaches get better within a few hours and can be treated with pain relieving medicines.
A severe and important headache can occur after a spinal injection. In young women having a spinal for childbirth it happens in around 1 in 200 or 300 spinals. It is much less common in older people having a spinal. This headache gets worse on sitting or standing and improves if you lie down. If this happens to you, you need to see an anaesthetist for assessment. If you are still in hospital, your nurses and the surgical team will organise this for you. If you have left hospital, you should seek help from your GP or by attending the emergency department.
Rare complications
Nerve damage – this is a rare complication of spinal anaesthesia. Temporary loss of sensation, pins and needles and sometimes muscle weakness may last for a few days or even weeks but almost all of these make a full recovery in time.
Permanent nerve damage is rare (approximately 1 in 50,000 spinals). It has about the same chance of occurring as major complications of having a general anaesthetic.
Frequently asked questions
Can I eat and drink before my spinal?
You will be asked to follow the same rules as if you were going to have a general anaesthetic. This is because it is occasionally necessary to change from a spinal anaesthetic to a general anaesthetic. The hospital should give you clear instructions about fasting.
Must I stay fully conscious?
Before the operation, you and your anaesthetist can decide together whether you remain fully awake during the operation or would prefer to be sedated so that you are not so aware of the whole process. The amount of sedation can be adjusted so that you are aware but not anxious. It is also possible to combine a spinal with a general anaesthetic.
Will I see what is happening to me?
A screen is placed across your body at chest level, so that you can’t see the surgery. Some operations use video cameras and telescopes for ‘keyhole’ surgery and some patients like to see what is happening on the screen. This is only possible if there is a spare screen.
Do I have a choice of anaesthetic?
Yes. Your anaesthetist will assess your overall preferences and needs for the surgery and discuss them with you. If you have anxieties regarding the spinal then these should be answered during your discussions.
Can I refuse to have the spinal?
Yes. If, following discussion with your anaesthetist, you are still unhappy about having a spinal anaesthetic, you can always say no. You will never be forced to have any anaesthetic procedure that you don’t want.
Will I feel anything during the operation?
Your anaesthetist will not permit surgery to begin until he/she is satisfied that the spinal is working properly. You should not feel any pain during the operation but you may be aware of movement or pressure as the surgical team carry out their work.
Should I tell the anaesthetist anything during the operation?
Yes, your anaesthetist will want to know about any sensations or other feelings you experience during the operation. They will make adjustments to your care throughout the operation and be able to explain things to you.
Is a spinal the same as an epidural?
No. Although they both involve an injection of local anaesthetic between the bones of the spine, the injections work in a slightly different way.
Where can I learn more about having a spinal?
You can speak to your anaesthetist or contact the pre-assessment clinic or anaesthetic department in your local hospital.
Questions you may like to ask your anaesthetist
1 Why is a spinal a good idea for me?
2 What benefits does it have over alternative techniques for me?
3 Who will give my anaesthetic?
4 Have you often used this type of anaesthetic?
5 Will I be unconscious and completely unaware during this type of anaesthetic?
6 Do I have any special risks?
7 How will I feel afterwards?
8 How will I feel afterwards if I don’t have a spinal?
You can find more information leaflets on the College website www.rcoa.ac.uk/patientinfo. The leaflets may also be available from the anaesthetic department or pre-assessment clinic in your hospital.
Risks associated with your anaesthetic
The following are leaflets about specific risks associated with having an anaesthetic or an anaesthetic procedure. They supplement the patient information leaflets listed above and are also available via the College website: www.rcoa.ac.uk/patientinfo.
■ Feeling sick.
■ Sore throat.
■ Shivering.
■ Damage to teeth, lips and tongue.
■ Damage to the eye during general anaesthesia.
■ Post-operative chest infection.
■ Becoming confused after an operation.
■ Accidental awareness during general anaesthesia.
■ Serious allergy during an anaesthetic (anaphylaxis).
■ Headache after a spinal or epidural injection.
■ Nerve damage associated with having an operation under general anaesthetic.
■ Nerve damage associated with a spinal or epidural injection.
■ Nerve damage associated with peripheral nerve block.
■ Equipment failure.
■ Death or brain damage.

